Gestational diabetes is prevalent among women and is increasing. The risk of being diagnosed with diabetes ranges from 2.7-16% according to age from 20-40 years old. The actual cause of gestational diabetes is the enormous hormonal changes that raise insulin resistance and reduce glucose availability for maternal tissues and organs. A low carbohydrate diet is a preferred choice for many healthcare providers for pregnant type 2 diabetics to help them manage blood glucose levels within the appropriate level. But is it feasible to do a low carbohydrate diet for a healthy woman who is newly diagnosed with gestational diabetes؟
This article aims to discuss the effect of pregnancy on maternal glucose metabolism and its impact on maternal and fetal health. Then, discuss the feasibility of implementation and the impact of a low carbohydrate diet on maternal hyperglycemia
Although low carbohydrate diets can effectively manage type 2 diabetes, they face challenges in implementation on pregnant newly diagnosed with gestational diabetes due to late diagnosis and adaptation difficulties. Studies haven’t found a widely applicable low carbohydrate diets method for pregnancy, but the author’s clinical experience shows benefits for committed patients who begin implementing the diet before pregnancy. In the author’s clinic, following low carbohydrate diets correctly (100-130g carbs) seems to reduce blood glucose, lower HbA1c, reduce complications, and help the mother reach full-term delivery successfully.
1.Introduction
Gestational diabetes is prevalent among women and is increasing. Yearly diagnoses of gestational diabetes increased from the period of 2016 to 2021 by 38%. The risk of being diagnosed with diabetes increases with age as a twenty-year-old female has a 2.7% chance of being diagnosed compared with a sixfold increase of 16% chance to be diagnosed with gestational diabetes at the age of forty (Martin and Gregory 2023).
The actual cause of gestational diabetes is the enormous hormonal changes that raise insulin resistance and reduce glucose availability for maternal tissues and organs. Of course, being metabolically healthy with an ideal body weight reduces the risk of experiencing gestational diabetes and hyperglycemia (Brown et al. 2016).
A low carbohydrate diet
A low carbohydrate diet is a preferred choice for many healthcare providers for pregnant type 2 diabetics to help them manage blood glucose levels within the appropriate level. But is it feasible to do a low carbohydrate diet for a healthy woman who is newly diagnosed with gestational diabetes? Given into consideration the increased prevalence of psychological issues among pregnant women with gestational diabetes (Morales Rodríguez et al. 2024).
As well as higher levels of stress, depression, and anxiety were observed in this group. Regardless of the potential benefits that a ketogenic or low carbohydrate diet can achieve, is it possible to change diet composition entirely in the last trimester of pregnancy, as the time for the pregnant woman to prepare herself for such a change emotionally and logically is too short? Such a change, to be accepted by the mother, should have time and a level of awareness of diabetes and its effect on herself and her upcoming child.
This article will discuss the effect of pregnancy on maternal glucose metabolism and its impact on maternal and fetal health. Then, the discussion will focus on low carbohydrate diets and their implementation effect on maternal hyperglycemia. Finally, the feasibility of implementing a low carbohydrate diet in women with gestational diabetes will be on the spot.
2.Conception
Pregnancy is the process that begins when a fertilized ovum is implanted in the uterus. This ovum continues to go through cell division and multiplication and increases in size until the delivery of a mature infant. The duration of gestational pregnancy is 38 weeks from the implantation of fertilized ovum until birth (Pascual and Langaker 2023).
To support embryo development into a fetus, throughout pregnancy until the delivery of a developed neonatal; different physiological and hormonal changes in the female body take place (Pascual and Langaker 2023). Failure to go through these changes properly can cause abnormalities in pregnancy development, which can cause future complications for both the maternal and fetus (Pascual and Langaker 2023). These changes include anatomical, physiological, and hormonal (Soma-Pillay et al. 2016). Vital organs increase in size and capacity to perform more functions. Blood volume increased by 20%, while plasma increased by 50%. Moreover, maternal organs and tissues, such as the heart, liver, kidneys, uterus, breasts, and thyroid gland, are enlarged. The growth and expansion of placenta size and hormonal secretions affect maternal nutrient metabolism, which is why both blood glucose and insulin levels increase (Brown et al. 2016)
3.Hormonal changes in pregnancy
During pregnancy the placenta plays a crucial role in macronutrient metabolic shifts in different trimesters and phases of pregnancy. These changes guarantee a continuous supply of energy-yielding nutrients to the placenta and the fetus (Kumar and Magon 2012).
The placenta begins to secrete human chorionic gonadotropin (hCG), which stimulates the corpus luteum to increase estrogen and progesterone during the first ten weeks (Kumar and Magon 2012). then the placental hCG drops as it begins to secrete placental estrogen and progesterone, which begins two months after conception (Brown et al. 2016).
Both estrogen and progesterone directly affect pancreatic beta-cell insulin production. leading to increased insulin blood concentration from conception until birth. This continued increase in insulin concentration increases insulin resistance in women with glucose intolerance (Kampmann et al. 2019).
Human chorionic somatotropin (hCS)
The dramatic increase of human chorionic somatotropin (hCS). also named human placental lactogen (hPL) (Kampmann et al. 2019), the diabetogenic effect of pregnancy appears more clearly (Brown et al. 2016). This effect makes pregnant women carbohydrate intolerant. It causes a rise in blood sugar if insulin secretion cannot cope with increased insulin resistance caused by hCS and prolactin secretion, which increases in the second half of pregnancy (Brown et al. 2016).
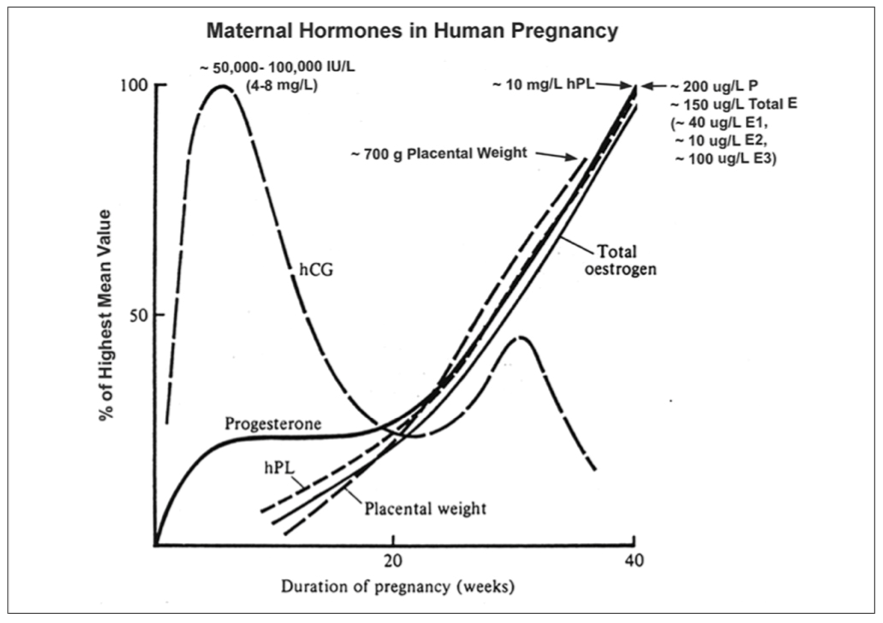
Figure 1:various hormone levels during pregnancy (Bajwa et al. 2011)
During normal pregnancy sensitivity to insulin is decreased to about 50-60% in maternal tissues. This insulin resistance advances during gestation in both healthy women and women with gestational diabetes (Kampmann et al. 2019). Insulin resistance starts in the second trimester (12-14 weeks) with a 39% reduction of insulin sensitivity and continues to rise until it beaks in the third trimester (34-36) with a 56% reduction of insulin sensitivity (Sharma et al. 2022; Soma-Pillay et al. 2016). These changes in cells’ insulin receptor sensitivity are overcome by an increase in pancreatic beta cells’ insulin production. Still, women with diabetes fail to cope with the demand for more endogenous insulin secretion during pregnancy, which leads blood sugar to rise (Kampmann et al. 2019).
4.Gestational diabetes
Gestational diabetes is a serious pregnancy complication in which healthy women who have never been diagnosed with diabetes before develop chronic hyperglycemia and hyperinsulinemia during maternity. Usually, the diagnosis of gestational diabetes is caused by long-term chronic insulin resistance before conception that leads to pancreatic β-cell dysfunction. This β-cell dysfunction impaired glucose tolerance for women with gestational diabetes and caused hyperglycemia (Plows et al. 2018).
Gestational diabetes is a common pregnancy complication. So that the International Diabetes Federation (IDF) estimates that gestational diabetes affects about 14% of pregnancies around the globe (Cho et al. 2018).
To screen for gestational diabetes, a glucose tolerance test is performed at the beginning of the third trimester, between 25 and 28 weeks of gestational pregnancy (Anon 2020).
Average fasting blood glucose
An average fasting blood glucose level is less than 95 mg/dL. Blood sugar after an hour of a meal or three hours after drinking the glucose solution should be less than 180 mg/dL, while postprandial glucose after two hours is to be lower than 155 mg/dL, and an average blood glucose level is lower than 140 mg/dL (Al-Husban et al. 2021).
But according to the American Diabetic Association. pregnant women should aim at a target of a fasting blood sugar 95 mg/dL or less, 140 mg/dL or less one hour after a meal, and the blood sugar after two hours better to be 120 mg/dL or less (Anon n.d.).
Having gestational diabetes increases risk factors for overweight and obesity and different metabolic syndrome diseases, such as cardiovascular disease, type 2 diabetes, macrosomia, and birth complications in the infant. Moreover. there is a longer-term risk of obesity type 2 diabetes, and cardiovascular disease in offspring (Plows et al. 2018).
5.Gestational Diabetes effect on the fetus
The rise of postprandial blood glucose above 180mg/dl after meals is high reading (Al-Husban et al. 2021).As 180mg/dl is considered the glucose kidney threshold in which nephron tubules fail to reabsorb all lost glucose to the bloodstream (Hieshima et al. 2020). This causes loss of water and potassium from the pregnant body. The excretion of glucose out of the circulatory system throws a urinary tract, increasing the risk of the maternal urinary tract and vaginal infection supported by reduced immune system function in pregnant women immune system. Moreover, the loss of water and salts caused by hyperglycemia increases the risk of dehydration, which adds more risk to the maternal body and fetus.
Hyperglycemia affects sleep quality by increasing nocturnal activity caused by increased urine output and reduced maternal bladder size. Lack of deep sleep increases stress and cortisol levels, which in turn increases fasting blood glucose and insulin secretion.
High glucose effect on fetal
Unfortunately. high maternal glucose levels are directly related to high fetal glucose levels. The fetus’s pancreas has difficulty managing and maintaining blood sugar below 250 mg/dL (Feige, Künzel, and Mitzkat 1977). Glucose values above 250mg/dl lead to dehydration in the mother and fetus, leading to a catastrophic increase in glucose-derived by an increase in glucagon blood concentration (Sapra and Bhandari, 2023). This increases the effort of the pancreas to reduce the blood sugar level. This justifies the increase and enlargement (hyperplasia and hypertrophy) of the pancreas beta cells of fetuses of mothers with high blood sugar (Holemans, Aerts, and Van Assche 2003).
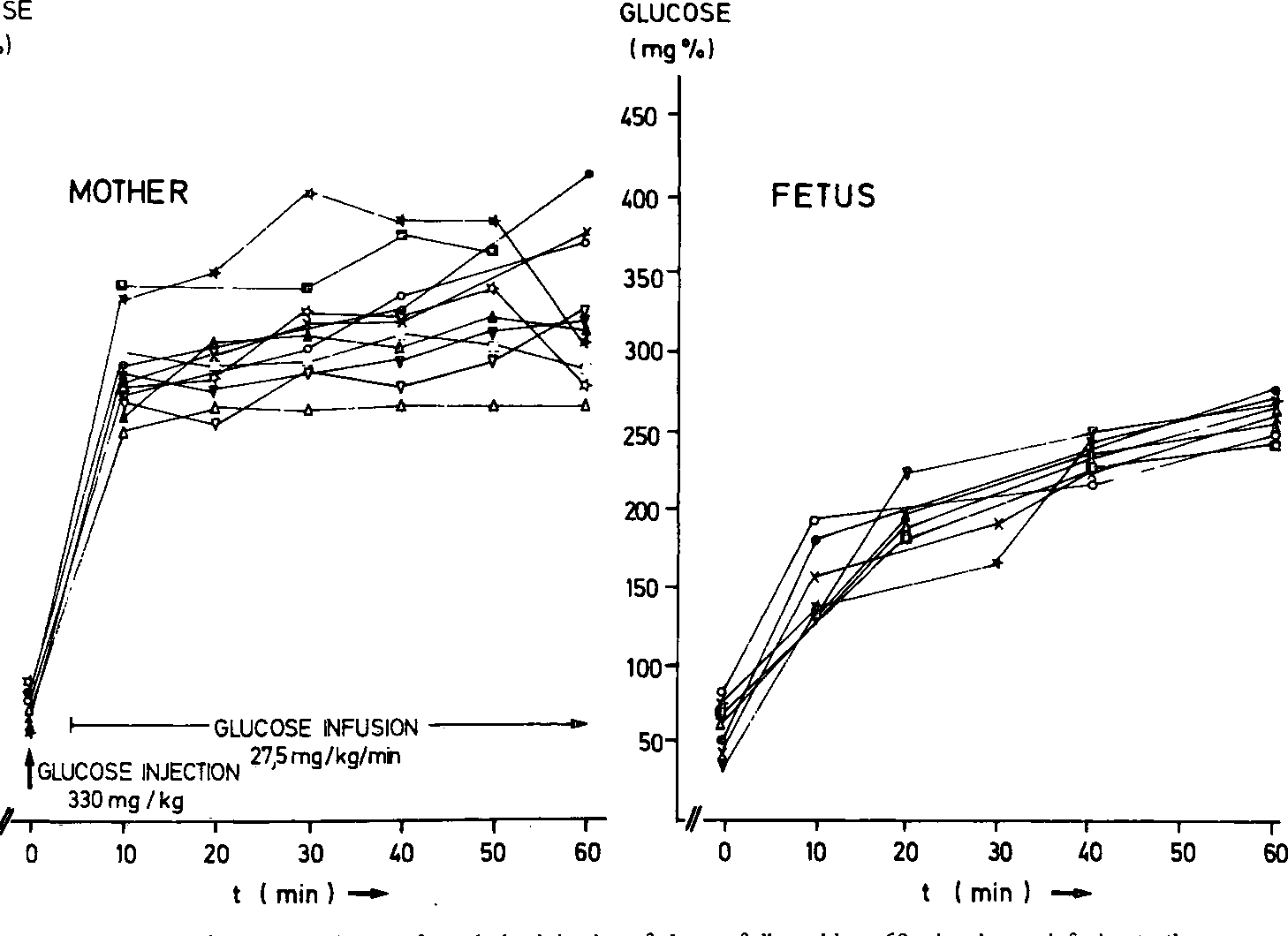
Figure 2: Maternal and fetal blood glucose after a bolus injection of glucose followed by a 60 min. Glucose infusion to the mother. After the injection of 330 mg/kg body weight glucose, a rapid increase of maternal blood glucose occurred within 10 min (Feige et al. 1977).
6.Low carbohydrate diet for controlling glucose in Gestational Diabetes
According to the American Diabetes Association (ADA). low carbohydrate diets are defined and classified as having a daily carbohydrate consumption of less than 130 g/day, or a percentage of carbohydrate less than 26% of total energy intake (TEI). Strict low carbohydrate diets and restricting carbohydrates were accepted methods for treating diabetes even before insulin discovery. Back then, glycosuria was eliminated by severe carbohydrate restriction to less than ten g/day or by performing a water fast until it was eliminated (Turton, Raab, and Rooney 2018).
A large observational study involving 1020 Europeans with outpatient type 1 diabetes reported that there is an association between an increased total carbohydrate intake (% of energy) and a higher potato carbohydrate consumption (g) and higher levels of HbA1c; on the other hand, HbA1c is reduced with increased vegetable carbohydrate intake(g) (Sapra and Bhandari, 2023).
Low carbohydrate diets
Low carbohydrate diets have shown promise as an effective approach for managing blood sugar levels in type 2 diabetes compared to other dietary approaches. (19)The American Diabetes Association recognizes this potential and includes low carbohydrate diets as an alternative approach for people with diabetes. However, close monitoring is necessary to ensure proper medication adjustments and potential reductions as needed.(20)
A systematic review was conducted on eight studies examining adults and children with type 1 diabetes who followed low carbohydrate diets (less than 45% of calories from carbohydrates (Turton et al. 2018). A review found heterogeneous outcomes, with only three studies reporting a significant reduction in HbA1c (average 1.3%). Other five studies showed stable blood glucose levels (20).
A systematic review recommended that future research investigate more potential consequences of low-carbohydrate diet interventions aimed at reducing HbA1c in insulin-dependent patients. An effective intervention should significantly lower HbA1c without increasing the risk of severe hypoglycemia. Additionally, other markers, such as total daily insulin use, BMI (body mass index, ≥25 kg/m²), and mean blood glucose, need to be studied (Turton et al. 2018).
The American Diabetes Association
Low carbohydrate diets have shown promise as a practical approach for managing blood sugar levels in type 2 diabetes compared to other dietary approaches (Wheatley et al. 2021). The American Diabetes Association (ADA,2021) recognizes this potential and includes low carbohydrate diets as an alternative approach for people with diabetes (Cucuzzella, Riley, and Isaacs, 2021). However, close monitoring is necessary to ensure proper medication adjustments and potential reductions as needed (Merrill et al. 2020).
7.Low carbohydrate diet for pregnant women with gestational diabetes
There are a lot of clinical complications associated with pregnant women diagnosed with gestational diabetes. These complications raise the chance of developing type 2 diabetes mellitus in the later stages of life to 60% chance.(21) Gestational diabetes.if left unmanaged during pregnancy, is related to a higher risk of developing risks that can lead to maternal and perinatal morbidity and mortality in some cases (22).
Failure to manage blood sugar harms offspring at birth and for a long time after. These adverse effects include perinatal morbidity stillbirth large for gestational age (LGA) babies, macrosomia birth, delivery hypoglycemia, Incidence of jaundice in newborns, perinatal deaths, birth injuries, Children born to mothers with gestational diabetes have higher risk of developing obesity and type 2 diabetes later in life (Brown et al. 2016). (23)
Low carbohydrate diets are suggested to help manage blood sugar. avoid maternal and offspring complications, and reduce postprandial blood glucose and hyperinsulinemia. A carbohydrate diet is a meal plan that reduces carbohydrate intake to less than 35–45% of total daily energy intake or total carbohydrate not to exceed 130 g of carbohydrate per day.(24)
When appropriately applied, this diet is highly effective in reducing postprandial hyperglycemia and hyperinsulinemia. Moreover, implementing low carbohydrate diets reduces fetal glucose exposure and fetal overgrowth (LGA) (24).
Cons and pros of low carbohydrate
There is a discussion among the medical teams about the cons and pros of low carbohydrate diet implementation. First different studies try to determine the minimum carbohydrate threshold to be consumed. Some studies try to push the minimum consumption not to be less than 175, while others tried to give around 130-165g of carbohydrates; in one study, a very low carbohydrate ketogenic diet was discussed to be given to pregnant with gestational diabetes with carbohydrate about (20-50grams/day). Other studies suggest that carbohydrate intake between 47–70% in pregnancy supports standard fetal growth patterns.(25)
In general. there is a lack of high-quality evidence that supports the use of a low carbohydrate diet for gestational diabetes blood glucose management (24). Moreover achieving a target carbohydrate intake of only 135 g/d was challenging (27). However, evidence demonstrates that carbohydrate restriction improves maternal glycemia (26).
In my clinical practice type 2 and type 1 diabetics who experienced miscarriage and stillbirth before have a high commitment to carbohydrate restriction in a low carbohydrate diet. Patients who do low carbohydrate diets correctly with about 100-130 grams of carbohydrates achieve results such as reducing postprandial blood glucose and HbA1c and successfully reaching the delivery date with fewer complications for the maternal and fetus.
8.Conclusion
In conclusion, despite the tremendous success of low carbohydrate diets in managing type 2 diabetes.In general, studies available could not find a procedure that can be implemented in a large group of populations that benefits glycemic control throughout pregnancy for women with gestational diabetes. Gestation diabetes is diagnosed in the last trimester of pregnancy. Which does not give the time for pregnant women to be prepared emotionally and logically for dramatic diet change. In my clinical practice type 2 and type 1 diabetics who experienced miscarriage and stillbirth before have a high commitment to carbohydrate restriction in a low carbohydrate diet. Patients who do low carbohydrate diets correctly with about 100-130 grams of carbohydrates better achieve results. Such as reducing postprandial blood glucose and HbA1c and successfully reaching the delivery date with fewer complications for the maternal and fetus.
References
12.Early Pregnancy Glycemic Levels in Non-Diabetic Women and Pregnancy Outcome: A Retrospective Cross-Sectional Study
- 17.Diabetes